Safe Weight Loss Surgery: What Patients Need to Know
Losing weight is hard. Maybe that’s why more than 1.9 billion adults globally are overweight, 13 percent of them obese. Almost half of the global population report that they’re currently trying to lose weight, but research has shown that the more diet attempts an individual makes, the more likely he or she is to gain weight in the future.
There are numerous reasons individuals fail at weight loss, from following a fad diet and avoiding exercise to drinking too much alcohol, consuming too many surgery and high-fat foods and not getting enough sleep. Even those who are successful at losing weight are likely to regain it, with research suggesting that roughly 80 percent of people who shed a significant portion of their body fat will not maintain that degree of weight loss for 12 months but instead regain, on average, more than half of what they lose within two years.
What’s the difference between overweight and obesity? The World Health Organization (WHO) defines overweight as a body mass index (BMI) greater than or equal to 25 and obesity as a BMI greater than or equal to 30. More than two-in-five adults worldwide are obese, and almost 10 percent of the globe’s inhabitants have severe obesity.
Being obese doesn’t only affect an individual’s appearance. Obesity is one of the leading risk factors for premature death and is a major risk factor for noncommunicable diseases, such as cardiovascular diseases, musculoskeletal disorders and metabolic disorders, the most common of which is diabetes. It also can cause increased physical limitations, bodily pain and fatigue and affect mental health. One study found that morbidly obese women were four times more likely to be depressed as women with a normal BMI.
All About Bariatric Surgery
When dieting and other weight loss interventions don’t work, some individuals turn to bariatric surgery. Often referred to as weight loss surgery, the goal of bariatric surgery is to modify the stomach and intestines to treat obesity and related diseases. Some weight loss procedures limit how much you can eat; others work by reducing the body’s ability to absorb nutrients and a few of them do both.
Although only a weight loss option for those who are morbidly obese, modern bariatric procedures have strong evidence of efficacy and safety, with complication rates lower than common operations, including gallbladder removal, hysterectomy and hip replacement. A majority of bariatric surgeries are done as a laparotomy, an open abdominal procedure with a large incision, or laparoscopically, meaning a minimally-invasive, camera-assisted abdominal procedure with a small incision.
Patients with a BMI higher than 35 have a less than one percent chance of reaching a normal body weight for a lasting period of time. Bariatric surgery can be performed on these individuals to help them not only lose weight but also reduce their risk of potentially life-threatening weight-related health problems. Qualifications for bariatric surgery in most areas include:
- BMI ≥ 40, or more than 100 pounds overweight
- BMI ≥ 35 and at least one or more obesity-related co-morbidities such as type II diabetes (T2DM), hypertension, sleep apnea and other respiratory disorders, non-alcoholic fatty liver disease, osteoarthritis, lipid abnormalities, gastrointestinal disorders or heart disease
- Inability to achieve a healthy weight loss sustained for a period of time with prior weight loss efforts
The American Diabetes Association recommends bariatric surgery be considered for adults with Type 2 diabetes who have a BMI greater than 35. It’s important to note, though, that chronic overeating can stretch the stomach and cause it to enlarge again, potentially canceling out the benefits of the surgery.
Benefits of Bariatric Surgery Beyond Weight Loss
According to the American Society for Metabolic and Bariatric Surgery (ASMBS), around 90 percent of patients after bariatric surgery experience improvement in related medical conditions and lose 50 percent of excess body weight and keep this extra weight off long-term. Those who have it tend to lose much more weight than people who get medical therapy for their weight loss – as long as they follow the recommendations for change in their diet and physical activity.
In large scientific studies, bariatric surgery has been shown to lower a person’s risk of death from any cause by over 40 percent. The average three-year weight loss for these surgery patients is 62 percent of excess weight.
Although weight loss is the most obvious advantage of bariatric surgery. Other benefits of weight loss surgery include long-term remission for type 2 diabetes, improved cardiovascular health and joint pain relief. Approximately 80-85 percent of patients experience remission of their sleep apnea one year after surgery, and individuals who underwent bariatric surgery had a 32.7 percent decrease in depression at the time of surgery and 16.5 percent decrease six to 12 months after surgery.
Safe Options for Weight Loss Surgery
The type of bariatric surgery that works best for a patient depends on several factors, including their general health, their health needs and their own preference. In this article, we’ll outline the four safest weight loss surgeries and the advantages of each.
Adjustable Gastric Banding
Probably the most simple surgery of the four with the lowest risk of complications, this type of procedure often is called lap banding because it involves the placement of a permanent silicone band around the stomach. During lap banding, a surgeon also inserts a port under the skin of the patient’s stomach, with a thin tube connecting it to the band. Typically performed laparoscopically, adjustable gastric banding can lead to loss of 40-50 percent of the patient’s weight.
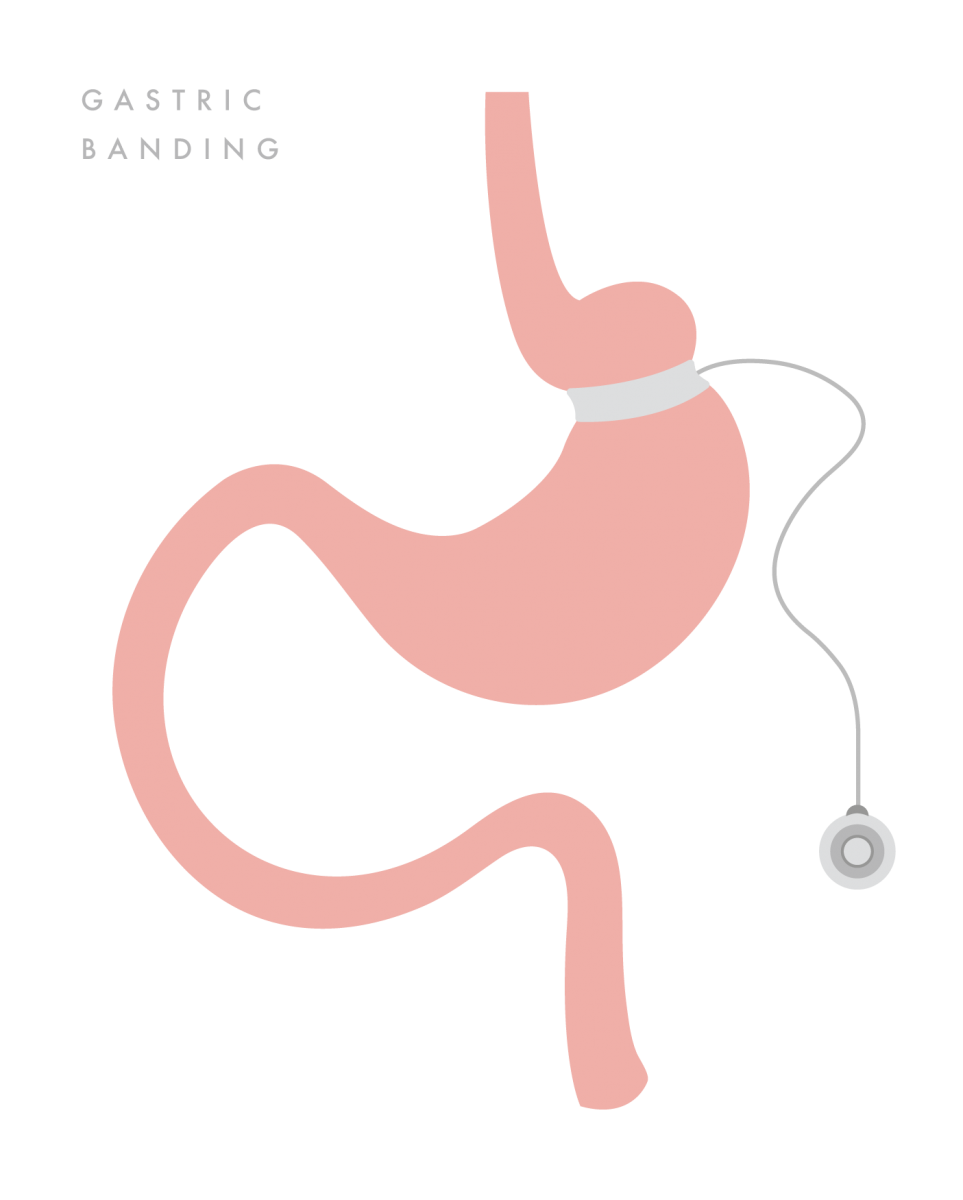
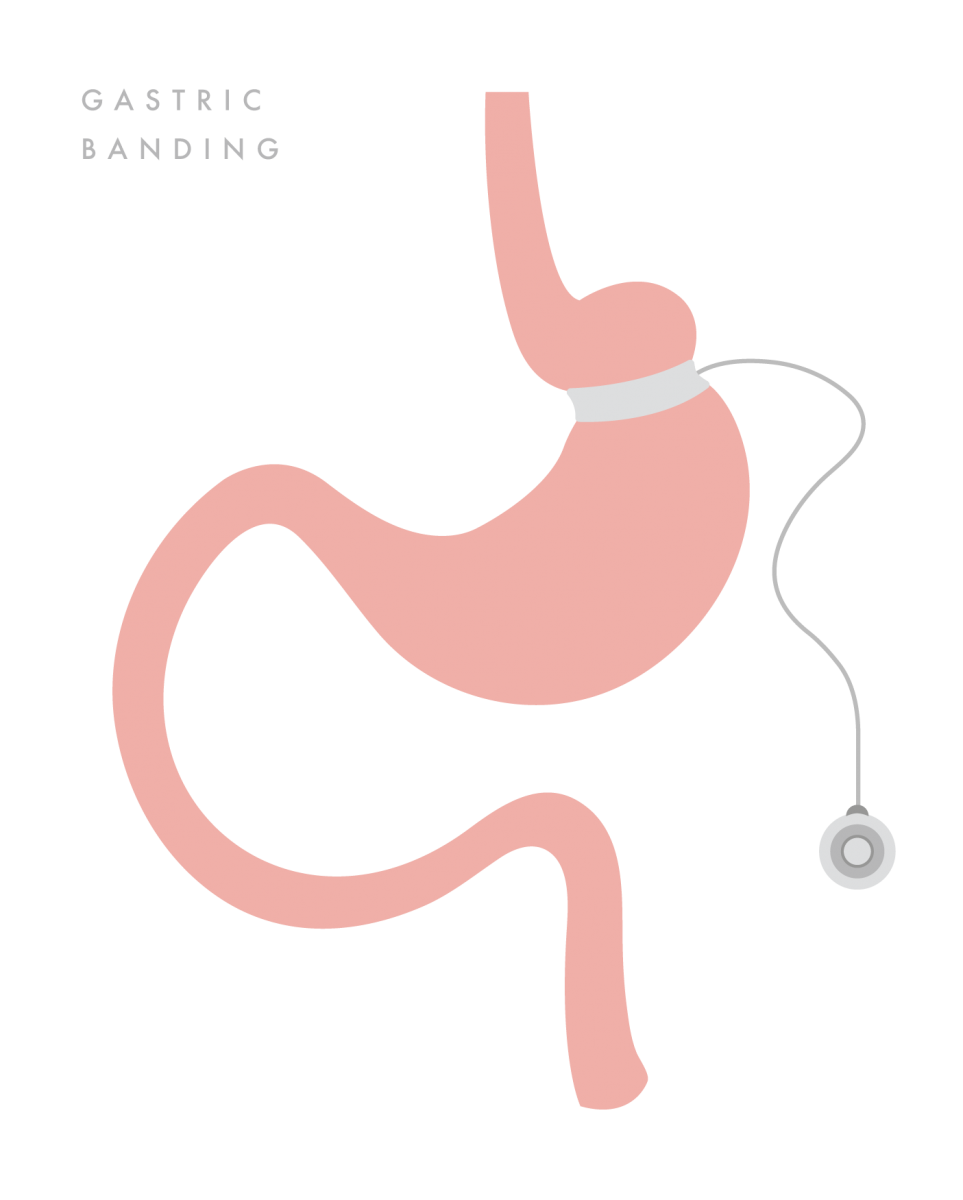
Benefits of laparoscopic gastric banding include:
- The possibility of long-term weight loss for those with obesity
- Relatively rapid recovery
- A smaller chance of wound infections and hernias after surgery
- Reduced risk of diabetes, high blood pressure, urinary incontinence and other conditions related to excess weight
- No loss of nutrient absorption
Sleeve Gastrectomy
Sometimes called gastric sleeve, this one-to-two-hour procedure is performed by dividing and removing approximately 80-85 percent of the stomach, the remainder of which is shaped like a sleeve or banana. It’s more complex than lap banding due to much of the stomach being removed. Gastric sleeve reduces the amount of food an individual can fit in his or her stomach, making them feel full sooner. The procedure doesn’t require any rerouting of the intestines, so it requires a shorter hospital stay than most other procedures. Patients who undergo a sleeve gastrectomy can expect to lose anywhere from 50-100 pounds – as long as they eat and exercise as instructed.
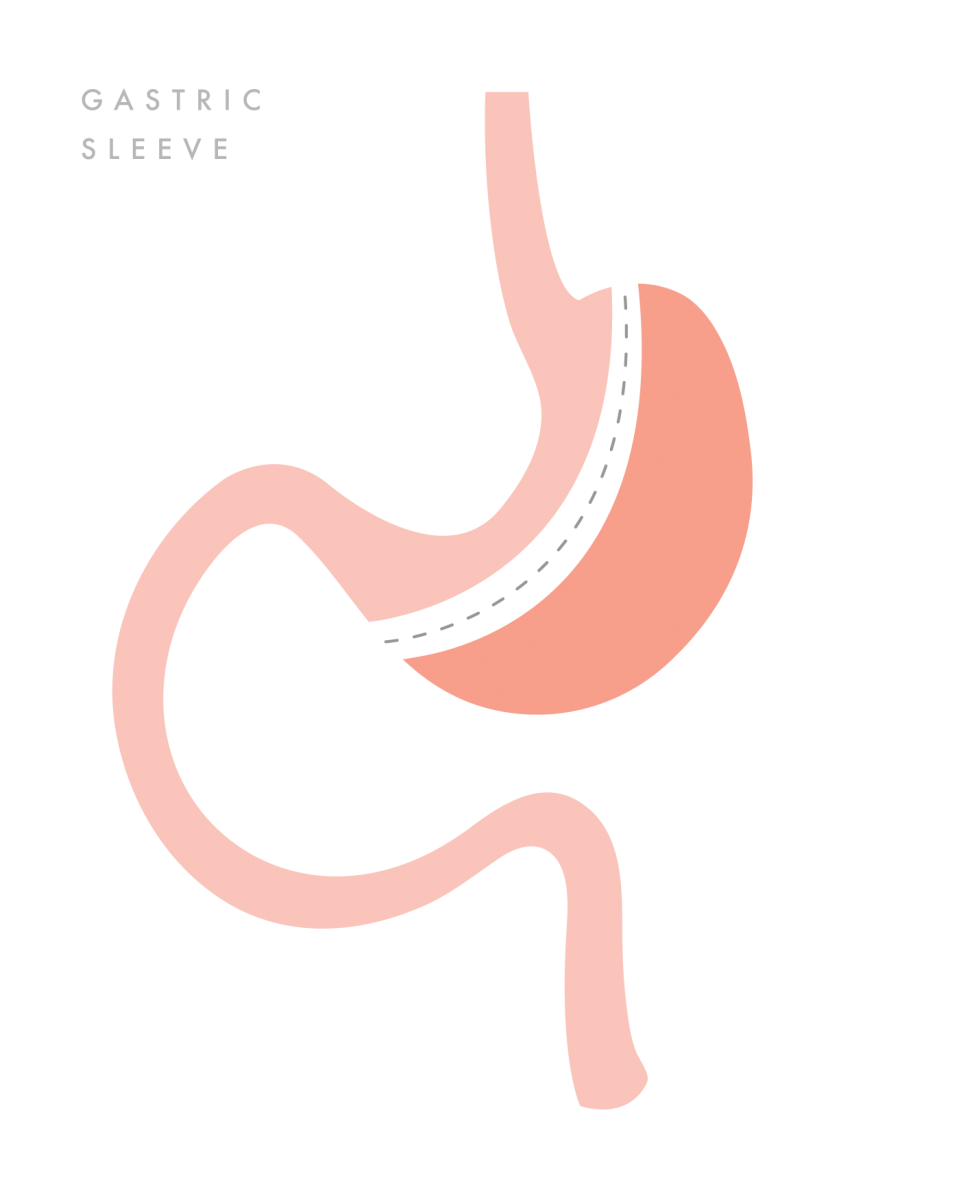
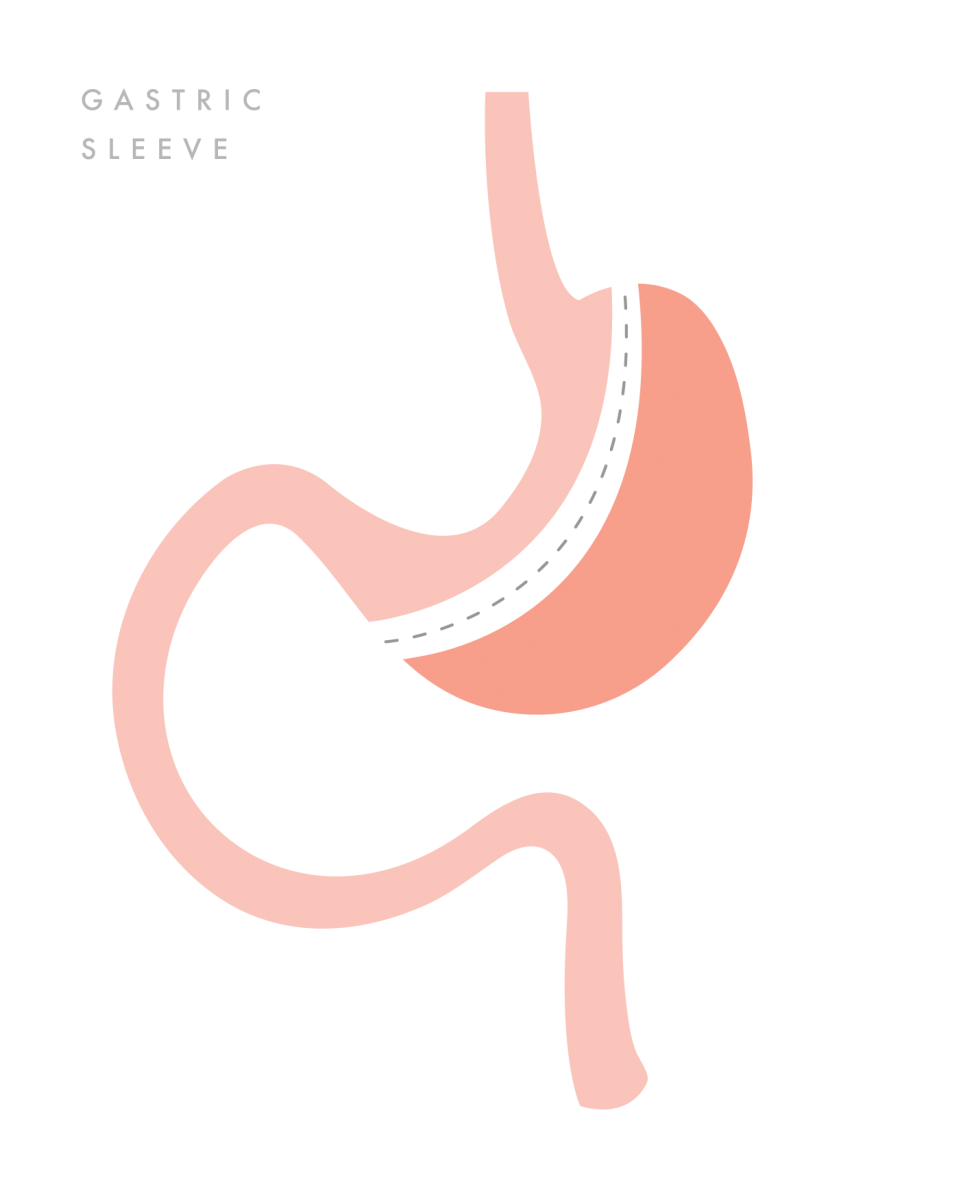
Benefits of sleeve gastrectomy include:
- A technically simple and shorter surgery time
- The ability to be performed in certain patients with high-risk medical conditions
- A first step for patients with severe obesity
- Use as a bridge to gastric bypass or SADI-S procedures
- Effective weight loss and improvement of obesity related conditions
Single Anastomosis Duodeno-ileal Bypass with Sleeve Gastrectomy (SADI-S)
A modification of the duodenal switch (DS) procedure, SADI-S is a newer bariatric operation in which sleeve gastrectomy is followed by an end-to-side duodeno-ileal diversion. It starts the same way as a sleeve gastrectomy, followed by the first part of the small intestine being divided just after the stomach. Then, a loop of intestine is measured several feet from its end and is connected to the stomach.
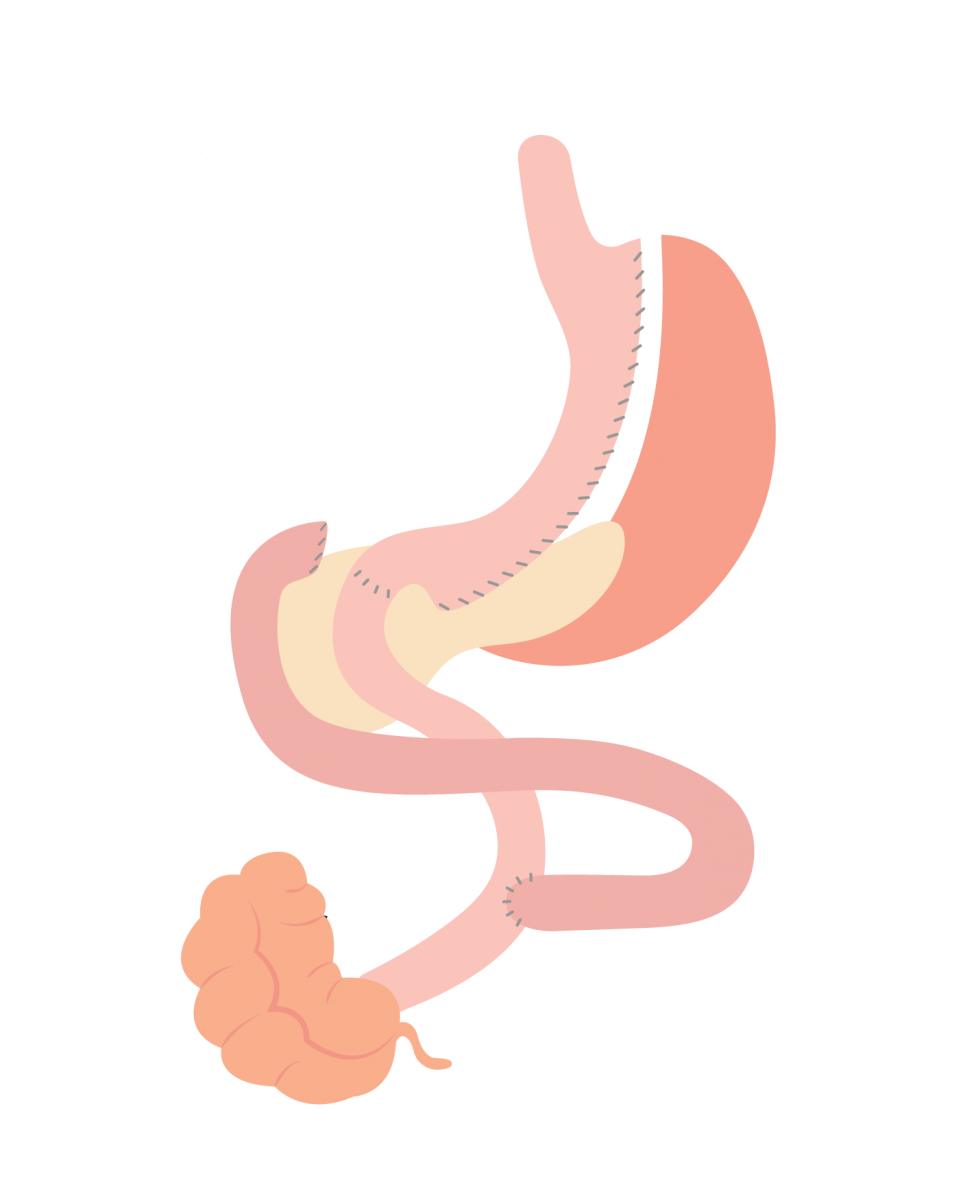
The most recent procedure to be endorsed by the ASMBS, it’s a shorter procedure than the DS and offers the benefits of a combined malabsorptive and restrictive bariatric operation. Often used for morbidly obese patients with an excessively high BMI, it’s performed laparoscopically through small incisions.
Benefits of SADI-S include:
- A highly effective option for long-term weight loss and remission of type 2 diabetes
- A simpler and faster procedure than gastric bypass to perform
- An excellent option for a patient who already had a sleeve gastrectomy and is seeking further weight loss
Roux-en-Y Gastric Bypass (RYGB)
Typically referred to as simply gastric bypass, RYGB is one of the most common bariatric operations and is performed by dividing the stomach to create a gastric pouch and surgically connecting the small intestine to the smaller stomach. The procedure, which is one of the best to improve or resolve diabetes, takes about two-to-three hours, changes hormones, bacteria and other substances in the gastrointestinal tract that may affect appetite and metabolism and often is not reversible.
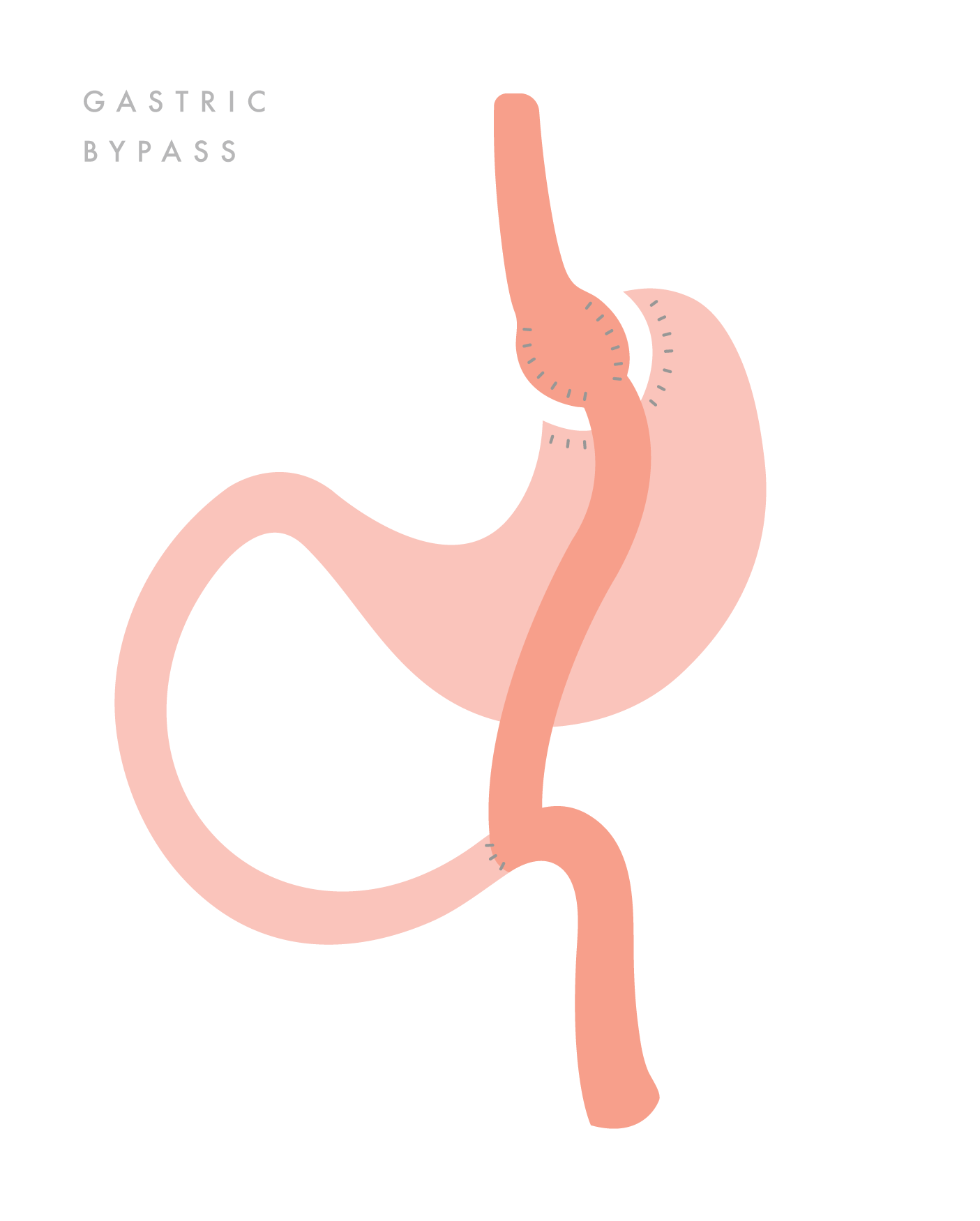
With gastric bypass, about half of a patient’s weight loss occurs in the first six months but may continue for up to two years post-operation. Studies have found that many people who undergo RYGB keep off most of the weight for ten years or longer.
Benefits of gastric bypass include:
- Reliable and long-lasting weight loss
- An effective procedure for remission of obesity-associated conditions
- A refined and standardized technique
About VIDA Bariatrics
Bariatric surgery by itself isn’t a long-term solution for weight loss. Patients must follow suggested dietary guidelines and avoid consuming too many calories.
No matter which type of bariatric procedure a patient selects, it’s crucial that he or she chooses an accredited surgery center with a board-certified physician experienced in weight loss surgery. The facility should have support staff that offers an education program and guidance on pre- and post-operation recommendations. Click below or above to start your 100% FREE Virtual Consultation with one of our board-certified Doctors.