The Complexity of Obesity & COVID-19
In the early days of the COVID-19 pandemic, obesity was identified as a risk factor for severe illness for COVID-19 sufferers. As time went on; studies continued to come out, citing the disproportionate toll of COVID-19 on people with overweight/obesity vs. those who had a healthy weight.
People with obesity (BMI ≥ 30 but < 40 kg) or severe obesity (BMI of ≥ 40 kg) were classified as having a higher risk of getting severely ill from COVID-19 and the risk of severe COVID-19 illness increases sharply with an elevated BMI. But why is obesity such a major risk factor for COVID-19, and how has this impacted those suffering from this disease?
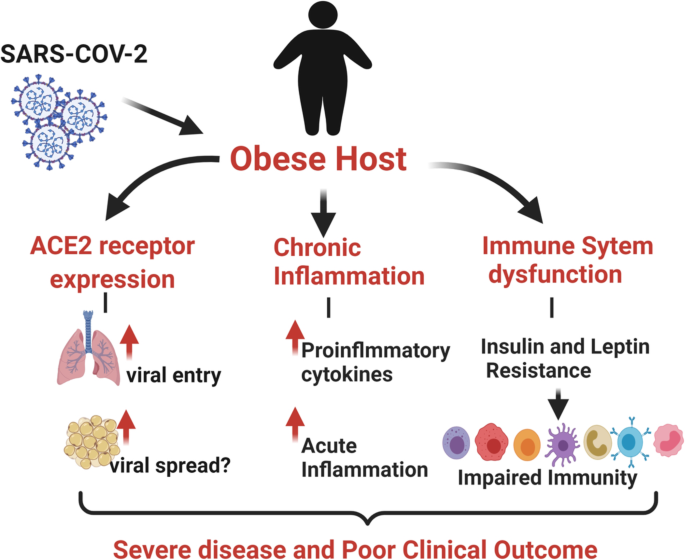
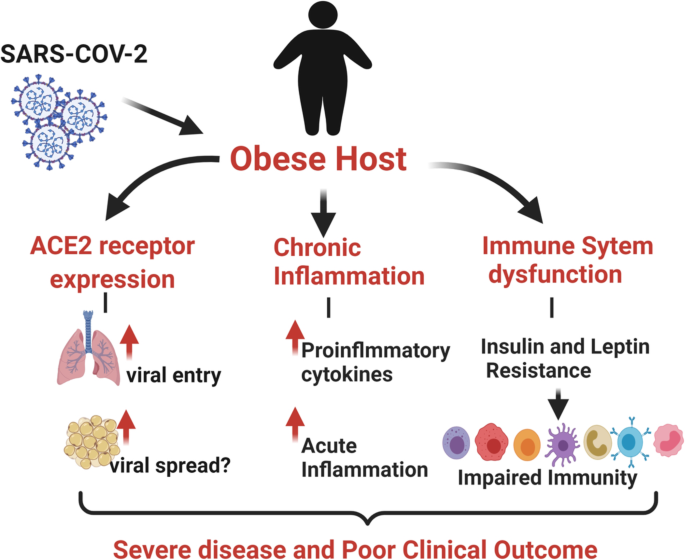
Image from here
Obesity, The Immune Response & COVID-19
Those patients clinically defined with obesity have impaired immune function and are already at an increased risk for severe infectious disease. Obesity already causes a low-grade activation of the immune response and has been associated with a chronic inflammatory state within the body. So when a patient with obesity is faced with an infection – the body will struggle to react in a positive way because it is already working within the body.
This same theory proves true when a patient that is overweight or obese who is already immune-compromised comes in contact with COVID-19. The body is often unable to compensate and fight off the infection, and the weakened immune system will give the COVID-19 the room it needs to infiltrate the body and trigger an inordinate inflammatory response. This weakened state creates more serious symptoms in patients with overweight or obesity than in those who are at a healthier weight.
Obesity, Preexisting Conditions & COVID-19
Having an impaired immune function from obesity is not the only reason COVID-19 raises the risk rates for people with obesity. Often, pre existing conditions exacerbate the problem and add to additional complications. Type 2 diabetes, which so often accompanies obesity, is a condition that can make COVID-19 symptoms worse. Preliminary studies have shown that about 25% of people who went to the hospital with severe COVID-19 infection had diabetes. Of those who had COVID-19 and diabetes, they were more likely to have serious complications or even die.
While there is not enough data to suggest that those with diabetes are more likely to get COVID-19 than the general population – the problem that occurs is that COVID-19 in those who have diabetes will have more complications from COVID. That, and many people with obesity are at risk for, or already have, type 2 diabetes which coupled with obesity is a very serious risk factor for COVID-19.
The COVID-19 and Beyond
According to the CDC, About 78% of people who have been hospitalized, need a ventilator, or died from COVID-19 were overweight or obesity. This high number begins to highlight the public health implications of higher BMIs and if the problem needs to be addressed on a deeper level, more specifically, why are there so many people with overweight and obesity in the United States.
“The COVID-19 pandemic has made us aware of the complex interactions of obesity with infectious diseases, and the gaps in our understanding of how chronic health conditions affect our immune responses to acute infection,” said Durga Singer, M.D., of the University of Michigan in Ann Arbor, Mich.
While scientists have shown that the chronic inflammatory state associated with obesity worsen the condition of numerous diseases – the public health implications are screaming louder. Has the obesity epidemic been a major contributor to some of the leading causes of death in the U.S come under new scrutiny by both the scientific community and the public at large? With COVID-19 shining a light on the disproportionate amount of deaths and illnesses from those with COVID-19 vs. those without, perhaps it is time to look at alternative methods of solving or approaching the obesity epidemic.